Pelvic Organ Prolapse FAQ
What causes Pelvic Organ Prolapse?
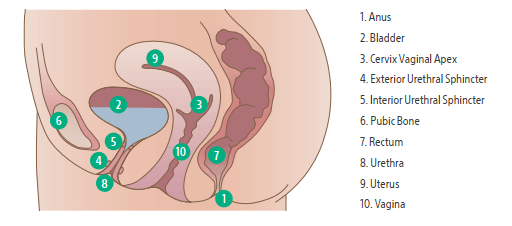
Pelvic organ prolapse occurs when muscles and ligaments in the pelvic floor are stretched to become too weak to hold the pelvic organs in the correct position. Potential causes include pregnancy and childbirth, aging and menopause, obesity, pelvic tumors, chronic coughing, chronic constipation, heavy lifting, prior pelvic surgeries or genetic factors.1
What are some symptoms of Pelvic Organ Prolapse?2
Pressure or discomfort in the vaginal or pelvic area, often made worse with physical activities such as prolonged standing, jogging or bicycling. Other symptoms include:
• Diminished control in the bladder and/or bowels
• A bulge near the opening of the vagina
• Painful intercourse
What are the treatment options for Pelvic Organ Prolapse?
Depending on the severity and the type of prolapse, your physician will discuss the different treatment options you may want to consider. Pelvic floor exercises to strengthen the pelvic floor, known as Kegels, may be adequate for mild cases.3 Another treatment option is a pessary, a ring-like device worn in the vagina to provide support for the organs that have fallen (or prolapsed). Pessaries are typically fitted by healthcare professionals. If symptoms are still bothersome and can’t be managed with a pessary or other
non-surgical options, surgery may be needed. All treatment options should be discussed with your physician.4
When is surgery recommended to treat Pelvic Organ Prolapse? What are examples of surgeries that are performed to treat Pelvic Organ Prolapse?
If non-surgical treatments do not provide sufficient relief of your symptoms and your pelvic organ prolapse continues to cause pain, problems with bowel and bladder functions or if it interferes with your sexual activity, you may choose to discuss surgical options with your doctor. The goal of any type of surgical treatment for prolapse is to repair the supporting tissue of the prolapsed organ or vaginal wall using either the patient’s own tissues or a surgical mesh. Surgeries can be performed either through the abdomen
or the vagina. Surgeries performed via the abdomen may be performed laparoscopically or through open abdominal incisions. It’s important to discuss all of your options with your physician to determine which treatment plan is most appropriate for your specific medical situation.
• Surgical procedures that use patients’ own tissues and ligaments to treat pelvic organ prolapse include Modified McCall culdoplasty, high uterosacral ligament suspension, uterosacral ligament fixation and sacrospinous ligament fixation.5
• Surgical procedures that use surgical mesh to treat prolapse via an abdominal incision include
sacrohysteropexy or sacralcolpopexy.6,7
• If a physician determines that the patient’s uterus is prolapsing into the vagina, the surgical removal of
the uterus (hysterectomy) may be recommended as a treatment option for pelvic organ prolapse.8
How is surgical mesh used in the treatment of Pelvic Organ Prolapse?
Surgical mesh is a medical device that is generally used to repair weakened or damaged tissue. In urogynecologic procedures, surgical mesh is permanently implanted to reinforce the weakened vaginal wall to repair pelvic organ prolapse.7
What types of materials may be used and what are the risks?
There are several surgical materials that could be used to facilitate your repair. These include a synthetic
polypropylene mesh or biologic grafts made of human dermis. The material will reinforce the vaginal wall
at the location of the pelvic organ prolapse. Potential Adverse Events associated with implanting synthetic mesh in pelvic organ prolapse procedures can be found below.
Please consult your physician to discuss the associated risk and complications for the specific surgical material you receive. Below is a list of potential adverse events for Boston Scientific’s pelvic organ prolapse
surgical material.
Potential adverse events, any of which may be ongoing, include but are not limited to: Abscess (swollen area within the body tissue, containing a buildup of pus), Adhesion formation (when a scar extends from within one area to another), Allergic reaction (hypersensitivity) to the implant, Bruising, Bleeding, Constipation, Dehiscence (opening of the incision after surgery), De novo detrusor instability (involuntary contraction of the bladder wall leading to an urge to urinate), Dyspareunia (pain during sexual intercourse) that may not resolve, Sexual dysfunction (difficulty with sexual response, desire, orgasm or pain); including the inability to have intercourse, Erosion into organs; exposure/extrusion into vagina (when the mesh goes through the vagina into other organs or surrounding tissue), Exposed mesh may cause pain or discomfort
to the patient’s partner during intercourse, Fistula formation (a hole/ passage that develops through the wall of the organs) which may be acute or chronic, Foreign body reaction (body’s inflammatory response
to the implant) which may be acute or chronic, Granulation tissue formation (reddish connective tissue that forms on the surface when a wound is healing), Hematoma formation (a pool of blood under the
skin/bruising), Hemorrhage (profuse bleeding), Infection, Inflammation (redness, heat, pain or swelling at the surgical site as a result of the surgery) which may be acute or chronic, Injury to ureter (the duct that
urine passes from the kidneys to the bladder), Scarring/scar contracture (tightening of the scar), Mesh contracture (mesh shrinkage), Tissue contracture (tightening of the tissue) Necrosis (death of living tissue in
a small area), Nerve injury (injury to the nerve fiber), Organ perforation (a hole in or damage to these or other tissues that may happen during placement), Pain: pelvic, vaginal, groin/thigh, dyspareunia-which may
become severe, Perforation or laceration of vessels, nerves, bladder, or bowel (a hole in or damage to these or other tissues that may happen during placement), Post-operative bowel obstruction (blockage that
keeps food or liquid from passing through the small or large intestines), Prolapse/recurrent prolapse (complete failure of the procedure), Vaginal shortening or stenosis which may result in Dyspareunia and/
or Sexual Dysfunction, Voiding dysfunction: incontinence, temporary or permanent lower urinary tract obstruction, difficulty urinating, pain with urination, overactive bladder, and retention (involuntary
leakage of urine or reduced or complete inability to empty the bladder). The occurrence of one or more of these complications may require treatment or surgical intervention. In some instances, the complication
may persist as a permanent condition after the surgical intervention or other treatment. Removal of mesh or correction of mesh-related complications may involve multiple surgeries. Complete removal of
mesh may not be possible and additional surgeries may not always fully correct the complications.
How likely is it that my prolapse will recur after surgery?
As with any procedure, some patients will have success while others will not. It is difficult to estimate your specific results. Your physician will explain all of your options and determine with you which treatment plan is most appropriate for your specific medical situation. Your physician will consider a number of factors to determine the likelihood of recurrence in your situation. The most appropriate treatment plan for you will be determined by taking many of these factors into consideration. The ultimate goal is to give you a lasting repair.
What if the surgical mesh comes through my vaginal wall at some point after surgery?
Exposure of the mesh (the presence of mesh material through the surrounding tissue) or mesh erosion (presence of mesh material within the organs surrounding the vagina) can occur following treatment of pelvic organ prolapse with surgical mesh. Treatment of these complications may include additional surgical procedures that may not correct the complication. Your physician will decide the best course of treatment for you if mesh erosion or exposure occur. Surgical mesh exposure and pain can occur years after initial mesh placement. Therefore, it is important to continue with your annual and other routine checkups and
follow-up care.8
If a surgical mesh is to be used in my surgical Pelvic Organ Prolapse repair, will my physician have
information on the product to be implanted?
Yes. You should ask your physician to give you a copy of any patient education information that he or she may have for the specific product used during your surgery, and keep it in your personal surgical file.
What should I expect after surgery?
Before your discharge from the hospital, you may be given a prescription for medication to relieve any discomfort you may experience. You will be instructed on how to care for your incision area. At the discretion of your physician, most patients resume moderate activities within 6 to 8 weeks, with no strenuous activity for up to 12 weeks to allow for healing.
What can I expect during recovery?
Every patient’s recovery experience is unique, and you should consult with your physician as to what he or she expects in your case. Your doctor will determine which kind of anesthesia will be used during your surgery, the length of time you may be hospitalized after the surgery, your need for additional medication following the surgery (for example antibiotics) and whether you will have to go home with a catheter (a flexible plastic tube that drains urine from your bladder). After undergoing prolapse surgery, you may
feel sore. Notify your physician immediately if you have pain with urination, bleeding, painful sexual intercourse, severe pain, defecatory problems or other problems after surgery.
Please consult with your physician on activities to avoid during recovery.9
Learn more at chooseyou.com.
Content is provided by Boston Scientific. Boston Scientific is dedicated to transforming lives through innovative medical solutions that improve the health of patients around the world.
REFERENCES
1. https://www.voicesforpfd.org/pelvic-organ-prolapse/ Accessed June 2021
2. https://www.voicesforpfd.org/pelvic-organ-prolapse/symptoms-types/ Accessed June 2021
3. https://www.voicesforpfd.org/about/physical-therapy/ Accessed on June 2021
4. https://www.voicesforpfd.org/about/pessaries/ Accessed on June 2021
5. Irvin W, Hullfish, K. Surgical management of vaginal vault prolapse. OBG Management. 2005 Nov;17(11):22-8.
6. https://www.webmd.com/women/guide/medical-treatments-pelvic-organ-prolapse Accessed June 2021
7. https://www.voicesforpfd.org/pelvic-organ-prolapse/surgery/ Accessed June 2021
8. Cheng YW, Su TH, Wang H, et al. Risk factors and management of vaginal mesh erosion after pelvic organ prolapse surgery. Taiwan J Obstet Gynecol. 2017 Apr;56(2):184-7.
9. Recommendations for Patients Considering Treatment for Pelvic Organ Prolapse with Surgical Mesh.
https://www.fda.gov/downloads/MedicalDevices/Safety/AlertsandNotices/ UCM262756.pdf. Accessed September 28, 2018.